New Hope in the Battle against Brain Tumors
The Brain Tumor Center at Beijing Puhua International Hospital (BPIH) manages as many, or more, clinical brain tumor cases as virtually any other such center in the world. The Center’s surgeons often operate on brain tumors that have been pronounced as “inoperable” by others. This facility provides surgical/non-surgical comprehensive treatment for brain tumors, providing optimum treatment options for these patients. The world’s most advanced treatments for brain tumor are offered at the Brain Tumor Center of Beijing Puhua International Hospital.
One of Asia’s top neuro-hospitals, BPIH keeps exploring advanced and effective therapeutic approaches for the benefit of brain tumor patients. Enormous achievements have been made by the excellent neurosurgery team at BPIH, which has become one of the only hospitals in the world that can offer the most advanced and comprehensive treatment to brain tumor patients.
“Working out better protocol to treat treatable diseases, and exploring new approach to treat “untreatable” diseases. I am always willing to do all what I can do to help each of my patients.”
—Dr. Xiaodi Han,
Neurosurgery Director & Vice-president of Beijing Puhua International Hospital

Dr. Xiaodi Han–Pioneer of Brain Tumor Treatment
Since working at the Neurosurgery Department of Beijing Tiantan Hospital, he was in charge of comprehensive treatment of glioma and various kinds of brain tumor treatments. He has worked at Alfred Hospital, Melbourne, Australia, and Wichita State University, Kansas, America. Subsequently, he has worked at the Neurosurgery Department of University of Rochester Medical Center where he was responsible for post-graduate research specializing in stem cell treatment.
Currently, Dr. Xiaodi Han is the Chief Neurosurgeon of Beijing Puhua International Hospital. He devotes himself to clinical work and teaching research of treatment for malignant brain tumor. He is ingenious at surgical treatment and comprehensive treatment for malignant tumor, which has brought him international recognition. In addition, he is a forerunner of stem cell research, both at home and overseas.
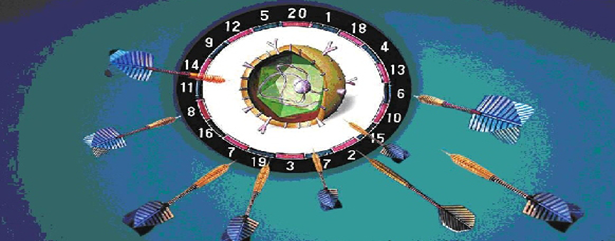
Surgery Candidates: comprehensive treatment protocol to remove tumor maximally and prevent recurrence:
Surgery: to remove tumor maximally while protecting functional area.
Intra-operative Radiotherapy (IORT): local radiotherapy to kill the residual cancer cells and prevent recurrence.
Intra-operative Chemotherapy (IOCT): local chemotherapy to kill the residual cancer cells and prevent recurrence.
Photon Dynamic Treatment (PDT): applied to highly malignant tumor to kill the residual cancer cells and prevent recurrence.
Non-surgery Candidates: effective and safe therapies to lessen suffering, prolong survival, and improve life quality:
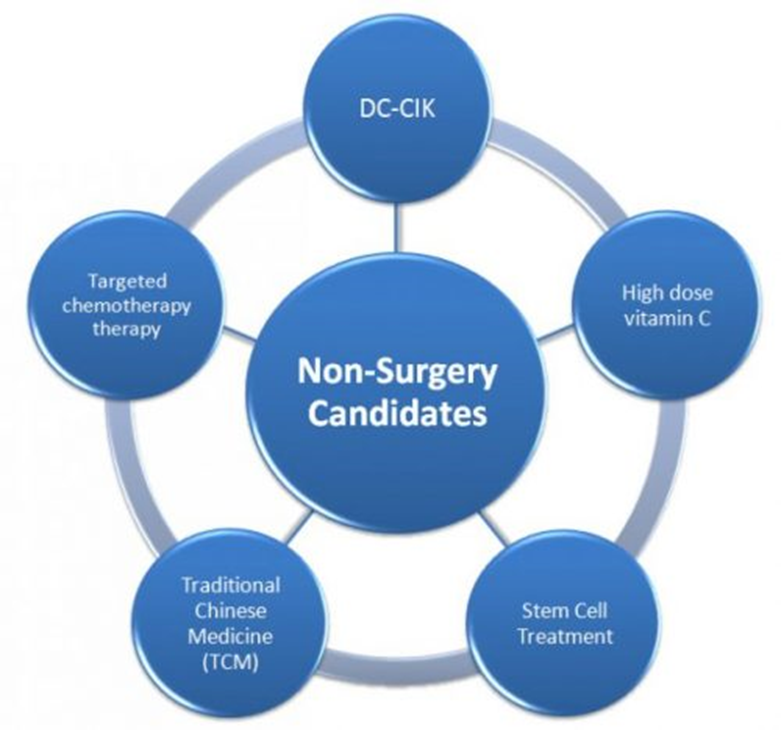
Targeted chemotherapy: based on genetic analysis, specific chemotherapy medicine to inhibit/kill tumor cell growth.
DC-CIK: CIK (Cytokine Inductive Killer-cell) and DC (Dendritic Cell) can fight tumor cells.
High dose vitamin C (IVC protocol): studies and clinical experience showed high dose vitamin C can inhibit cancer cell growth and improve patient’s overall condition.
Traditional Chinese Medicine (TCM): improving the patient’s overall condition by improving immune system and decreasing the toxicity of other therapies.
Surgery

Strengths of the Beijing Puhua International Hospital Neurosurgery Program
Brain surgery is obviously a serious subject, entailing both risks and expenses. Below are some of the more prominent risks and how they are managed and contained by the BPIH neurosurgery team.
1. Complications or Failures of Surgery: Beijing Puhua International Hospital is a neurologically-specialized & fully-licensed general hospital that works in coordination with the famous Tiantan Neurological Hospital in Beijing. The neurosurgery team utilizes the latest skills and works in a culture rich in both tradition and experience. In planning surgery, the neurosurgery team analyzes each case individually, adopting the optimal methods, thus minimizing risks and optimizing outcomes.
2. Loss of Function: A patient’s quality of life quality after surgery is always of top concern. Therefore, prior to the surgery, and during, the clinical team will always do its best to protect the patients’ post-operative neurological function. In this way, optimal post-op functions for every case are protected and safeguarded.
3. Tumor Recurrence: Even though most tumor tissue can be identified and removed during neurosurgery, some tumor cells may escape detection. If left behind, such residual tumor cells may survive and grow. To reoccurrence, intra-operative radiotherapy and intra-operative chemotherapy are utilized to eliminate the residual tumor cells. This approach can not only prevent reoccurrence of cancer in a highly efficient and effective manner, but it also avoids the suffering and side-effects of traditional whole-body radiotherapy and systemic chemotherapy.
Intraoperative Radiation Therapy (IORT)
&Intraoperative Chemotherapy (IOCT)c

What are IORT & IOCT?
Intraoperative Radiation Therapy (IORT) delivers concentrated radiation treatment to the tumor bed during surgery. This advanced technology helps to eliminate hidden populations of residual tumor cells: cells which might otherwise remain around the edges of the tumor bed, and later lead to recurrence. IORT reduces the need for EBRT (External Beam Radiotherapy) Treatment by provide a targeted radiation “boost” during the surgery.
Intraoperative chemotherapy (IOCT, such as with a localized BCNU wafer) delivers a concentrated dose of chemotherapy to the tumor bed during surgery. By eliminating side effects and remote toxicity, this technology is able to deliver up to 110 times more chemotherapy to the tumor than is possible by traditional systemic chemotherapy.
Advantages of IORT and IOCT
1. Maximum effect. Delivers a concentrated dose of radiation and chemotherapy to a tumor site immediately after a tumor is removed, which help to destroy the microscopic tumor cells that may be left behind. While the tumor site is typically at high risk for recurrence, traditional EBRT and chemotherapy requires a recovery period after surgery, which may leaves microscopic amount of tumor cells in the tumor site for longer.
2. Accurate targeting/Spares healthy tissues and organs. During IORT/IOCT, precise tumor-killing dosing is applied to suspicious tissues while shielding healthy tissues or structures that might have been be damaged using other methods. This allows a higher combined radiation and chemotherapy dose to be delivered to the tumor bed, while sparing healthy surrounding tissues. Critical organs such as the lungs or heart can also be protected from the effects of systemic radiation/chemotherapy.
3. Shortened treatment times. IORT/IOCT may help some patients finish treatment and get back to their lives quicker by reducing the need for additional EBRT or chemotherapy (typically given over five to six weeks). The IORT/IOCT treatment itself takes only about four to five minutes during surgery.
In the long-term clinical application of this technology on brain tumors, extremely good results have been demonstrated over the past 14 years. This combination therapy has been used in over 8,000 tumor cases, and initially was mainly utilized for treating breast cancer. Beijing Puhua International Hospital is one of the first facilities to apply this technology to an initial cohort of glioma patients, and has treated 126 cases of brain tumor cases as of this writing.
Photodynamic Therapy (PDT)
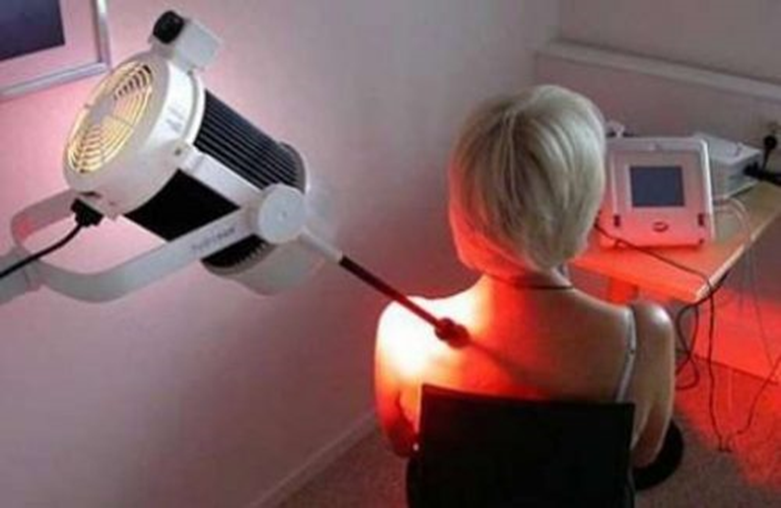
Photodynamic Therapy (PDT) (sometimes called photo-chemotherapy), is a form of phototherapy using nontoxic light-sensitive compounds that are exposed to selective wavelengths of light, whereupon they become activated and toxic to targeted malignant and other targeted tissues. PDT has been proven to kill bacteria, fungi and viruses, and is popularly used in treating acne. It is used clinically to treat a wide range of medical conditions, including wet age-related macular degeneration (AMD) and malignant cancers, and is recognized as an effective and selective treatment strategy that is both minimally invasive and minimally toxic.
PDT is mainly used at Beijing Puhua International Hospital to treat malignant brain tumors. While there are some limitations, this method is showing very good results.
Targeted Chemotherapy
Based on genetic analysis, specific chemotherapy medicine is selected to inhibit/kill tumor cells and thus control or eliminate tumor growth and/or recurrence.
Based on the genetic analysis of the tumor tissue, a specific chemotherapy medication may be given. This medication is one that blocks the growth of tumor cells by interfering with specific targeted molecules needed for a specific tumor’s growth (rather than simply interfering with cell division, as with traditional chemotherapy. Targeted cancer therapies offer the promise of being both more effective than current treatments and also less harmful to normal cells.
.
DC-CIK Immunotherapy
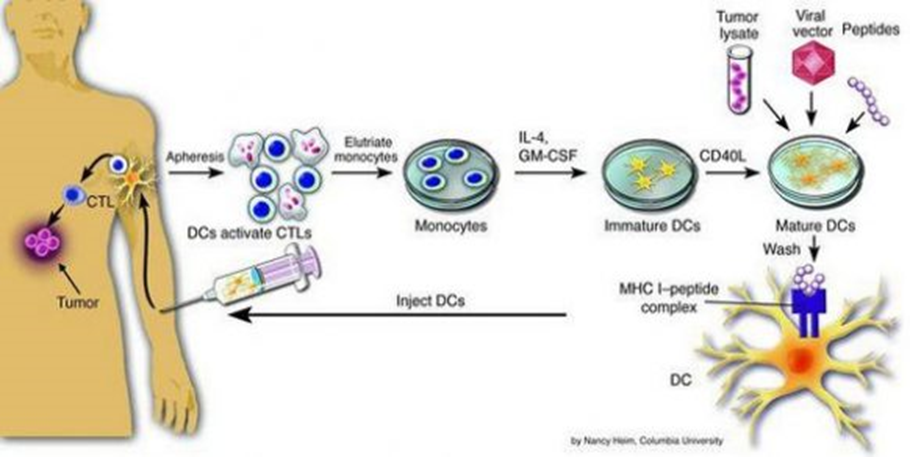
DC-CIK are methods used to fight cancer cells by augmenting the patient’s own immune system.
CIK (cytokine-induced killer) and DC (dendritic cell) therapy belong to the category of “adoptive cell therapy,” which utilize cultivated CIK and activated DC cells to fight abnormal cells, such as in tumors. Normally, the number of DC & CIK cells existing in body is very small, and insufficient to effectively fight against a given cancer. In DC-CIK therapy, these cells are isolated, sensitized to the tumor antigens, amplified at least 1,000 times, and then re-infused back into the patient’s body via IV infusion, where they potentiate the immune system to attack and help to eliminate the tumor.
High Dose Vitamin C (IVC protocol)
Cancer patients tend to be depleted of vitamin C: when vitamin C is given by intravenous infusion, cancer patients’ quality of life may be improved significantly, with benefits including increased energy, less nausea and vomiting, and improved appetite. No severe side effects due to IVC have been observed.
IVC protocol is employed at Beijing Puhua International Hospital as an effective and safe supportive therapy for cancer patients: many patient’s benefit from this elegant therapy.
Traditional Chinese Medicine(TCM)
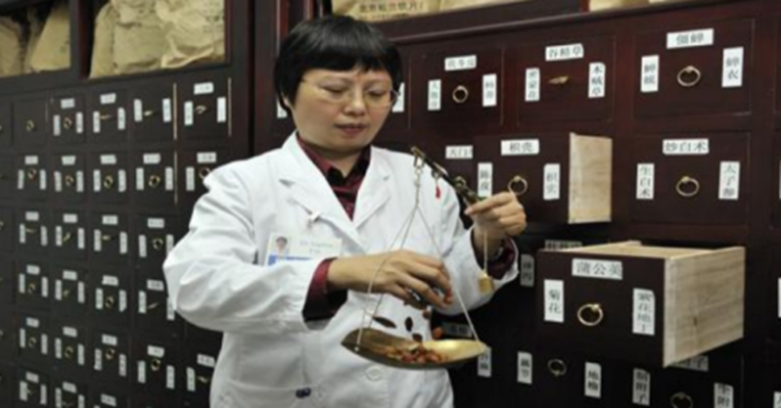
TCM is a safe and effective supportive treatment option used in conjunction with other treatment modalities. Many Chinese herbs have strong immune-enhancing effects, and can both enhance the effects of chemotherapy, radiation therapy, surgery, and other modalities while reducing toxicity and side-effects. Traditional Chinese herbs can be given orally, by IV infusion, or injected to the tumor feeding vessels with the help of DSA (digital subtraction angiography) guidance.