Stereotactic Minimally Invasive Brain Repair brings hope for patients with seizure disorders
It is well known that, currently, the incidence rate of epilepsy is approximately 20-50/100,000 worldwide. This means that tens of millions of people in all corners of the world suffer from this disorder and while treatments are available, not everyone can benefit from them.
The current range of anti-epileptic drugs and treatments focus on minimizing the symptoms by reducing the number of seizures that manifest but do little to alleviate the root cause. These treatments are generally only effective in around 70% of patients leaving 30% of Epilepsy sufferers out in the cold.
It is for this reason that Beijing Puhua International Hospital has pioneered the minimally Invasive Brain repair procedure.
Treatment Principle of Stereotactic Minimally Invasive Brain Repair
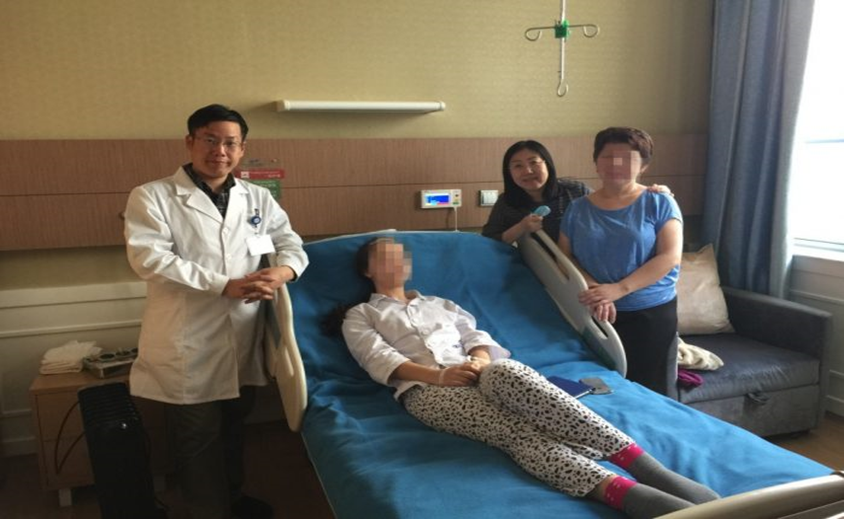
Stereotactic positioning allows a surgeon to map the human brain in three dimensions and pinpoint the afflicted area to within less than 1mm. Once positioned, single or multiple lesions and affected areas can be acted upon with a minimal effect to the surrounding tissue which has significantly improved the results seen by intractable epilepsy patients.
The hippocampal amygdala complex is a part of the Papez loop of the limbic system. It’s functions are closely related to human emotion, cognition, memory, verbal expression, smell, etc. Hippocampal sclerosis can easily lead to the formation of an epileptogenic zone, in which the amygdala and hippocampus can also play an amplification role to epileptiform discharge. The surgery resects, thereby completely disconnecting, the zone which not only reduces the excitability of epilepsy caused by surrounding strengthening structures but it also weakens the epileptiform discharge conduction pathway and improves the dysfunction of the limbic system.
Advantages of Stereotactic Minimally Invasive Brain Repair for Selected Seizure Disorder Patients:
1. Minimizes the footprint left by the surgery by greatly reducing the effect on surrounding tissue.
2. Extreme Precision that is accurate to 1-2 mm, with precise 3-D localization.
3. Increases efficiency by reducing the time on the operating table as well as increasing positive outcomes
Equipment Support used during Stereotactic Brain Surgery

Remebottm is currently the world’s most advanced neurosurgical-aided positioning system, and most often applied in seizure-disorder surgery and other surgical environments requiring ultra-high accuracy. Of the two Remebott systems in China, one is at Beijing Puhua International Hospital.
The Remebottm integrates an operation planning and navigation systems with robot-assisted positioning devices to greatly improve on the limitations of traditional brain surgery, making it a less invasive, more effective and less time consuming alternative.
Case Study
On 4th April 2016, an 18-year-old Kazakhstani patient suffering from an intractable seizure disorder, successfully underwent EEG-Guided, minimally invasive, stereotactic brain surgery and multipotent cell implantation at Beijing Puhua International Hospital (BPIH). Following this extremely precise ablative procedure, the patient has been seizure free and off of her previous anti-seizure medications. The patient’s mother described her daughter as having been offered a “second chance to live.”
The patient’s general condition prior surgery
• She suffered from daily paroxysmal limbs convulsions for 6 years, experienced improvement after drug therapy, but significant side effects limited this rate. Her seizures returned after going off of her medications.
• No anatomic abnormality was found in a brain MRI.
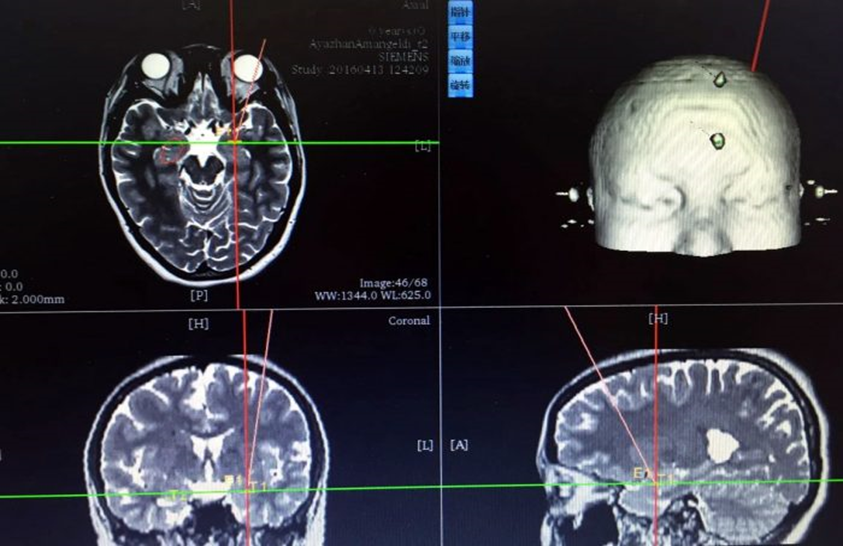
• However, EEG revealed abnormalities diagnostic for a seizure disorder.
Surgical Planning
Precise stereotactic localization data, uploaded to computer for robotic-guided ablation.

Dr. Lu preparing the robotic arm and patient.

Dr. Lu taking EEG readings from deep within the patient’s brain, followed by precision-guided radio-frequency ablation of the precise focus of the seizure disorder. The tiny residual skin incisions can be seen below, and will soon be hidden beneath the patient’s hairline.
EEG comparison: before and after radiofrequency
Before Radio-frequency Ablation (Above)
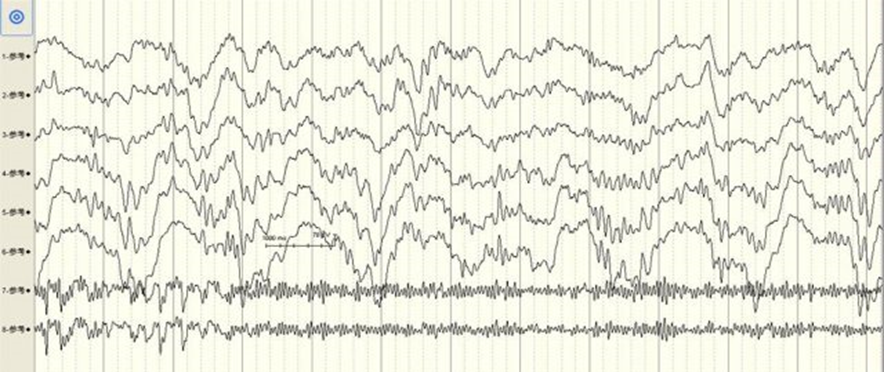
After Radio-frequency Ablation (Above)
Postoperative Condition
• Post-operative CT-imaging showed no intracerebral hemorrhage or complications;
• No seizures have occurred following the treatment, and the patient remains symptom-free whilst also being off of drug therapy.